Rebecca Sauer is a critical care nurse and local mosaic artist. She lives in Coronado with her husband, David, and her son, Andre. She flew to New York City to work in the intensive care unit of New York Presbyterian Hospital of Lower Manhattan during the COVID-19 outbreak. These are her diaries.
WEEK 1.
Sunday, 4/19/20
I’m in New York, and it’s surreal. All week I haven’t been able to believe I was going, and now, I can’t believe I’m actually here. I had done everything I could to prepare Andre, my seven- year-old sweet son for my leaving. A few nights earlier, I had held him in my arms in the big bed as he cried hard, sweating, and begging me not to go. I felt like a ghoul.
Why was I doing this? Nursing has never been a ‘higher-power’ type calling for me; I don’t have a Florence Nightingale complex. All week since announcing my plans, I’ve been getting the whole, “hero/angel” bit. It has made me absolutely cringe with discomfort. I’m neither.
I have the mouth of a sailor, the sense of humor of an 11 year old, am outspoken often to my detriment, and have faults too numerous to count. My husband, David deserves to be dipped in bronze and immortalized in song for putting up with me.
So again, why? Why am I leaving a family that needs me, to help strangers, and very possibly get infected? I’m overweight and have asthma. Covid-19 would probably be a death sentence. I’ve felt irresponsible, reckless, and foolhardy, but definitely not heroic. How can I explain my compulsion to go?

How can I explain that, where I work, they’ve cut back on elective surgeries to the extent that there’s practically no work to be done? All in preparation for a surge that, thanks to aggressive and early isolation and social distancing, hasn’t really hit yet. How can I explain that I’ve been antsy, twiddling my thumbs, marinating in the news and Facebook, not sleeping well, and just overeating out of anxiety and boredom? How can I explain my sense of aimlessness, purposelessness, and the feeling like my skills are going to waste here? The action is elsewhere, most urgently in New York City, and I feel like I just need to be there, plain and simple.
It’s where I should be right now.
Critical care nursing fulfills several needs for me. It’s unbelievably challenging at times, physically, emotionally, and intellectually. I need that stimulation. It gives me a sense of purpose and usefulness. Like I’m not just taking up space and wasting a carbon footprint. Forget Sudoku. I’d rather solve a puzzle that saves someone’s life, tweaking IV medications, adjusting someone’s airway, figuring out that the patient is crashing for a reason unseen by the naked eye, but that can be deduced by a series of actions, tests, skills, and experience.
I like the intimacy. I like being able to put a patient at ease when they’re at their most vulnerable. To me, it’s an honor. To comfort a family through the worst time of their entire lives- what could be more of a privilege? And to be there for fellow colleagues in their moment of desperation; that’s the calling. I can’t ignore it.
I want to go- feel compelled to go because they need help. And why shouldn’t it be me? (By the way, most of my colleagues think I’m nuts. They’re worried about me and don’t think I should risk it.) To each her own I guess when it comes to motivations. Luckily, I have a few closer ones who are behind me one hundred percent.
At the Jetblue check-in, it all started to close in on me. David heard my breathing quicken and could see the tears forming over the top of my mask. I had reassured him earlier that I had every intention of keeping it together for Andre. We feared that Andre would pick up on my emotional state. No dice. I began to hyperventilate slightly, and that started the sweats. I was starting to melt down. Andre noticed and came over to me, putting his little arms around me. “You’ll be okay, Mommy” he said.
The roles had reversed. He’d had his meltdown, and seemed to understand that now, I needed mine. As Andre comforted me, a sharply dressed man in line behind me offered kind and encouraging words. I had explained my situation to the ticket agent so she wouldn’t think I was bananas, and the man had thanked me for going to New York to help. When Andre and David and I sat down at a table to eat a little lunch together before parting, I told David about the kind man and his words, to which Andre piped up, “maybe he was looking for a date.”
Yeah, kid. Probably.
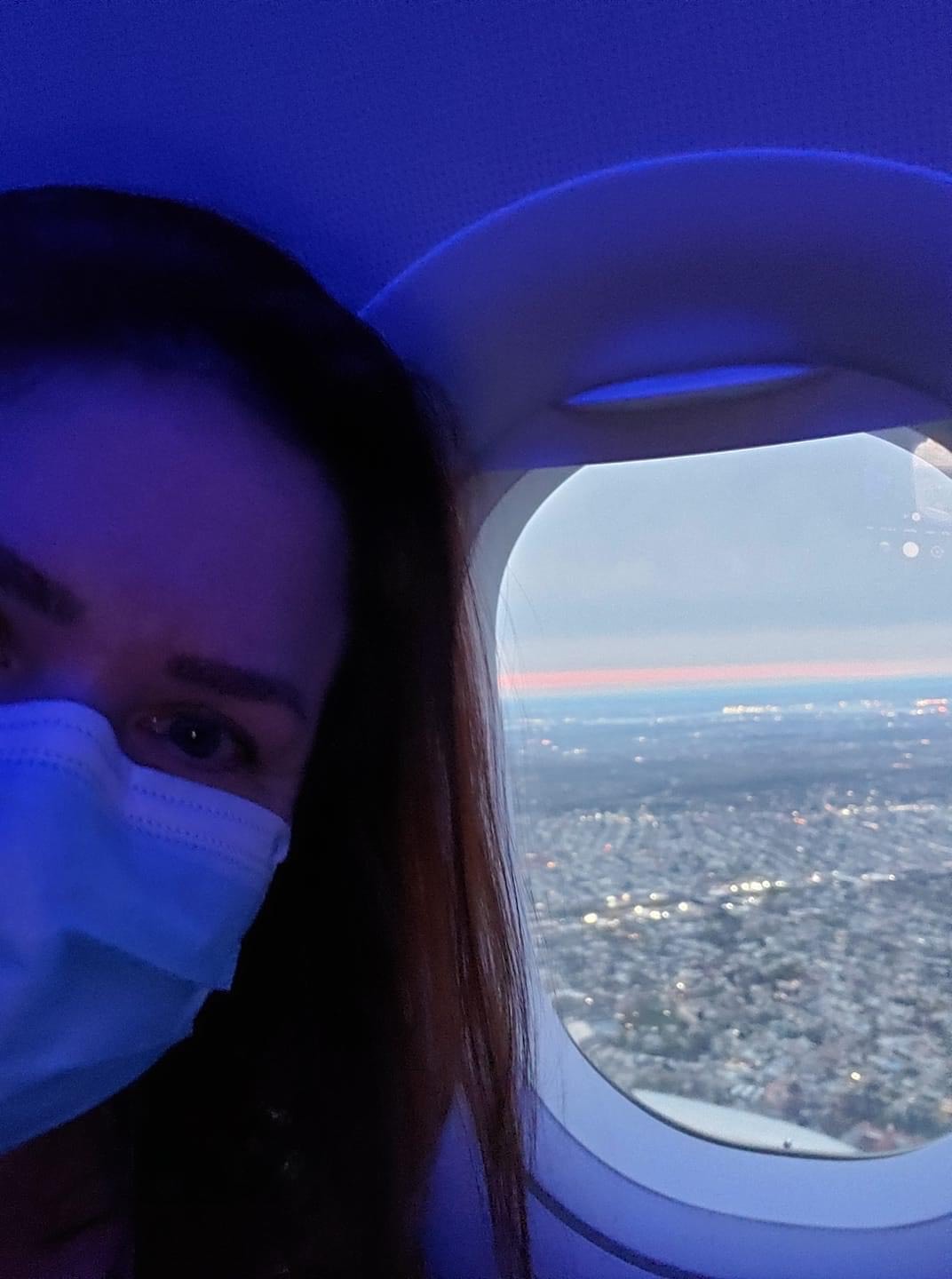
After an extremely pleasant flight with about 10 other people on board, some of whom were also healthcare providers, I got into my Uber for the trip from JFK into lower Manhattan, the night clear and brisk. I’d seen video of the Empire State Building, its upper third lit up in red and pulsing like a heartbeat- a tribute to healthcare workers. When it came into view I couldn’t help but choke up to see it in person.
I feel humbled being here. And disoriented, anxious, insecure and scared. Scared of buckling under the sheer physical stress of the job. Afraid I won’t hold up under all the PPE, which sucks to wear at the best of times. Afraid that I’ll pass out from dehydration from sweating, the hypercarbia that ensues when you wear an N95 mask for an entire 12-hour shift, rebreathing your own exhaled C02. I know of a nurse who passed out mere hours into her shift, having to get tested and sent home.
I don’t want to be a liability instead of an asset. I’m afraid of getting claustrophobic, of vomiting, of having a panic attack. I’m not prone to that, but anything can happen in this kind of high stress circumstance. Afraid I’ll screw up. These patients are SO fragile, they have to be chemically paralyzed to keep their vital signs stable. They can’t afford for me to be slow, or incompetent, or incapacitated.
My apartment is furnished and fully-equipped. It’s in Tribeca, a fantastic neighborhood in lower Manhattan, and my building is right on the Hudson. I got in at 9pm, and was grateful to find a 24-hour deli a block away. As I was looking for the deli, I still managed in my fatigue, to get slightly lost. Unconsciously, I found myself singing ‘’Me and Julio Down by the School Yard,” by Paul Simon. For one thing, I was walking past a school yard. Laughing to myself, I sang:
I’m on my way…
I don’t know where I’m goin’
I’m on my way, takin’ my time, but I don’t know where
Goodbye Rosie, Queen of Corona…
The queen of Corona, indeed. Oh, and my middle name is Rose. Could this be my new nickname? Anyway, I found the deli, and got a bagel with smoked trout. Even though my hands still stink after washing them like Lady Macbeth, it was worth it.
Monday, 4/20/19
Today I walked most of the way to my hospital, New York Presbyterian of Lower Manhattan. It’s a nice walk of just under one mile. About 95% of storefronts are closed and shuttered, so it’s unnaturally quiet. You can imagine how this neighborhood must bustle with vehicular and foot traffic; the Freedom Tower and WTC memorial are only about 4 blocks away.
The relative quiet was broken by a street construction crew. A worker complained about a pipe being too shallow, and his coworker responded with an authentic New York, “Fuggetaboutit!” I grinned under my mask in childish glee.

My walk takes me through the heart of Tribeca, and to my delighted surprise, through the small park that surrounds City Hall, home of audacious pigeons and fat brazen squirrels looking for a handout. Administering the handout today was Ron, whom I now think of as The Squirrel Whisperer. A lifelong Tribeca resident, he told me that feeding the squirrels is his therapy. While they ate out of his hand, sometimes scampering up his pant legs, he told me interesting details about the neighborhood and its architecture.

It was great. When he ran out of nuts, he told me he had to go to another park to feed “the professionals.” Apparently those squirrels sit on his lap. I love fuggetabout it guy. I love Ron. I love Tribeca. I love New York.
Tuesday, 4/21/20
I didn’t go out today. The weather report called for rough windy thunderstorms with hail. They kept saying it was going to hit any moment. I absolutely adore wild weather, and it’s something I miss, being in Southern California, so I was psyched. We did get some rain, wind and a couple of lightning flashes, but it was somewhat of a letdown.
I set my alarm for 6:55pm, and went up to the roof. I had heard the tribute to the essential workers the evening before, but nothing prepared me for hearing and seeing it from the 19th floor. At 7pm in New York, the people go wonderfully, loudly, joyfully goofy. They bang pots and pans, howl like wolves, shout, blow air horns, car horns, whistles, and generally whip up a cacophony. It was hard to not get choked up.
Elderly folks and little kids join their parents, shouting, “I love you, doctors and nurses!” They sustain the clamor for about five minutes, and it’s hard not to fall in love with them. I felt moved beyond belief, and for the first time, like I really am doing the right thing, and should be here, and am here for the right reasons. It’s the first time I’ve felt a sense of calm resolution in my purpose.
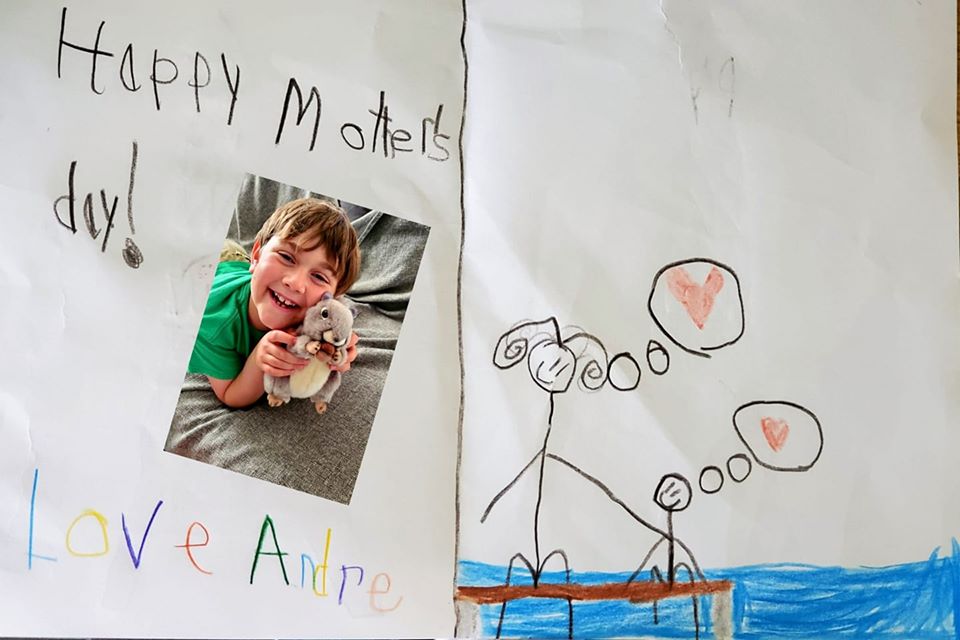
It’s still incredibly hard to not be able to hold Andre in my arms. He’s a pretty emotionally-attached and cuddly little guy. I’ve been video calling with them multiple times a day. Even in San Diego, I have to often say goodnight to him over the phone on days when I’m working, so it doesn’t seem that abnormal. He seems happy and his normal self. It’s still hard to not be able to mommy him in person, and to help comfort him through the distress of a loose tooth (Andre’s kryptonite). I know it’s hard for David as well. He’s teaching via Zoom and working on his master’s degree. I shopped like crazy and left them in a clean, well-stocked apartment. Still, I know full-time daddying is hard. I know that David is extremely worried about my welfare, but to his credit, he has supported me throughout this endeavor.
Wednesday, 4/22/20
Not much to report today. I start my online orientation tomorrow. It was a beautiful day today, clear and crisp with blue skies, but cold- in the low 40’s. I made my way to the neighborhood Whole Foods (any money I make from this contract will go right to them). But I need to get good food- fruits and veggies to keep myself healthy for what I’m about to go through. I can’t just eat bagels and smoked fish, as much as I’d like to.

The highlight of my day was meeting three- year-old Cooper and his lovely parents on the rooftop deck. Coop had a drum and drumsticks, and contributed to the din very nicely. The neighbor who comes out to the deck and howls, let out a “YABBA-DABBA-DOOOO” tonight. I love them all, and am determined to do my very best by them.
Thursday, 4/23/20
Today I went to my hospital for the first time so I could get my badge. The hospital looks somewhat old and dated, and a far cry from Coronado or La Jolla. The other nurses I’ve spoken to, both of whom work at different hospitals, have warned me about what I can expect. Old equipment, lack of equipment, and questionable dynamics between medical professionals. Patients unimaginably sick. It’s not my first rodeo. I’ll do whatever I can with whatever they have.

I began my online orientation. It took all day to complete computer modules. I spoke with one of my managers, who seems very nice. The peak of this initial surge appears to have passed. To put it into perspective, NY has gone from over 700 deaths/day, to over 400 deaths/day. I see it as having gone from an unmitigated catastrophe, to a mere disaster. They were bringing out a body to a hearse as I was leaving the hospital. At least it was a hearse, and not the 18-wheel refrigerator truck parked outside.

Make no mistake, it is a disaster, and these workers are whipped. They’re so tired. PTSD will be rampant- epidemic when this all calms down.
One of the reasons I hate the whole, “hero/angel” thing, is that, although well-meaning, it’s dehumanizing. We’re not fictional idealized characters, we’re actual people. We’re people who haven’t been trained to encounter anything remotely on this scale, but who have been thrust into it nevertheless. We’re people with feelings, who can only take so much. We’re people who have families that we’re terrified to infect. We’re people who get justifiably angry when we’re cheated out of protective equipment, and expected to just keep going in and taking it, as if signing up to be a nurse was to sign up to be a martyr. We’re people who are angry at being treated as disposable, sacrificial, and expendable. We are doing the best we can to protect a public, in many cases, from itself, and enduring some vicious verbal abuse while doing so.
Friday, 4/24/20
Today I finished my online orientation. Unfortunately, I’ve been so jet-lagged, I ended up nodding off halfway through the presentation. I spoke with a UCSD colleague who’s working at another hospital here. The other day, they ran out of oxygen. Let me repeat that: a hospital ran out of OXYGEN! She’d never heard of anything like that before, and frankly, neither have I.
I’m nervous about tomorrow. I haven’t worked anything like this before.
In the movie, “The Right Stuff,” Alan Shepard (played masterfully by Scott Glenn) sits in his Mercury capsule, ready for the countdown that will launch him into space. He says into an open mic, “Dear Lord, please don’t let me f#@% up.” That about sums it up.

WEEK 2.
Saturday, 4/25/20
It was an eerily quiet and calm first shift. I’d expected the 9th circle of Hell, but it seems like that eased up in about the last week or so. A week ago, New York finally saw less than 500 deaths per day. It’s hard to know the true numbers. Of course the conspiracy theorists opine that the number is inflated, but in truth, it’s probably pretty accurate- maybe even higher. We may never know the exact number, but hundreds upon hundreds a day is unspeakable. That we are becoming inured to that, is a testament to how altered our world has become. I continue to maintain that it’s improved from being an unmitigated catastrophe, to a mere disaster.
New York Presbyterian is a private hospital system that includes Columbia and Cornell- the bigger flagships. The Lower Manhattan location is a smaller outpost with the feel of a community hospital, and is driven by PA’s, not residents. Technically, I’m in the ICU float pool here, but since there’s only one ICU, I happily have a home base.
It is tucked into the southeastern onramp to the Brooklyn Bridge, on the edge of Chinatown. There is a beautiful old copper-roofed orange brick firehouse across the street with a huge Chinese tiger on the garage door. It reminds me so wistfully of the House of Dragons, my one-time home away from home in Philadelphia. I now have another reason to feel sentimental about Chinatown firehouses, and loved watching the guys in their turnout gear, playing street hockey in the preternatural stillness.

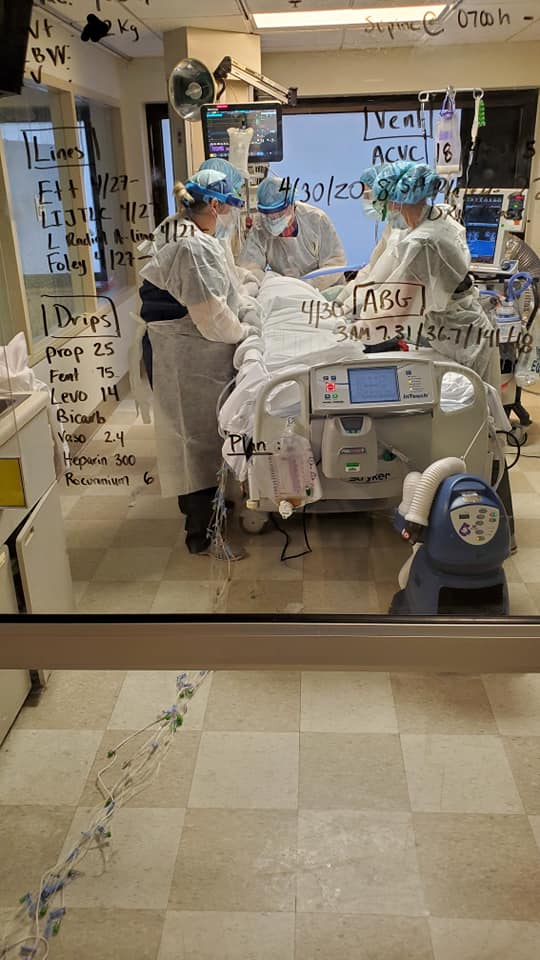
The unit itself is interesting. Physically, it’s worn and faded. Not the state-of-the-art I’m used to in La Jolla, or as flat-out shiny and full of art installations as Coronado. The layout is like a capital “H,” but with a few more connecting horizontals. The two long parallel corridors are the patient rooms, big glass boxes essentially.
In normal times, they would be visually separated from each other by curtains on the common glass walls in between, but those curtains have been removed, so you can see down and through the whole aisle of rooms at a glance. This is imperative, because when you’re in head-toe PPE and in a room and you need something, you want someone to see you waving right away. People are VERY good about visually checking each other regularly. You don’t want to have to rubberneck to get attention.


There are plenty of staff now that the travelers are all here. I only had one patient today with my preceptor. She was a sick patient for sure, but one that I could have taken paired with another one if they’d needed it. I didn’t see nursing assistants (although I think they have them) but what I did see were med-surg nurse travelers who are assigned to the ICU as helpers. I thought that was amazing.
There are fewer patients than just a week ago, when there were two patients in each single room. Today only one room had two patients. Almost every patient in the ICU has Covid-19, and almost everyone is very, very sick. To minimize the amount of time clinicians have to venture into a patient’s room, the IV pumps and CRRT machines (a continual non-stop form of dialysis for patients too critical to withstand big fluid shifts) sit outside the patient’s rooms in the hallways. Each pump requires about 3 lengths of IV tubing to reach the distance. It’s a huge tripping hazard in the room when in PPE, so you have to move about carefully. I’m no ballerina, so I have to be vigilant and tread purposefully.
My patient today was my age, only a few months older. Ventilated, sedated and on a IV pressor drip to keep her blood pressure stable, in spite of a ton of sedation, she was easily arousable–not a good feature when on a ventilator. If a patient is not well sedated, they’ll become desynchronis with, or fight the vent. Having a tube down your throat and a machine forcing you to breathe against your own body’s rhythms is panic-inducing. The urge to rip out the tube is irresistible and most, if not all have to be restrained for their own safety. Agitation also uses up metabolic reserves that the patient doesn’t have. The problem with over-sedation is that Propofol (aka, “the Michael Jackson drug”) is fatty. It’s looks like whole milk. The patients who are on this medication for too long have extremely elevated lipid profiles, which is problematic.
All the meds have side effects and adverse effects. Nothing is without risk. Even being intubated for too long can lead to tissue breakdown in the mouth and throat, and in the usual world, after ten days to two weeks, the patient would receive a tracheostomy and wean off the vent that way.
These patients aren’t weaning, however, they’re dying. They’re developing microscopic blood clots that occlude blood flow and therefore, can have impaired function to their lungs, brains, hearts, kidneys, and everything else. I heard about a patient somewhere who lost a leg due to Covid-related clotting. So you put them on blood thinners. And that causes other problems.

My lady today was on 60% FiO2. Room air is 21%. So by rights she should have terrific blood oxygen levels. Nope. Her blood oxygen, or SpO2, should have been 99-100%, but it was 95%. Normal on room air, not good on 60%. And then we laid her flat to turn her. Sedated critically ill patients need to be turned every two hours at minimum to prevent pressure ulcers. No matter how terrific the air mattress, they have to be turned. Pressure ulcers can kill. It’s a constant battle in the ICU. Nothing is worse for creating pressure ulcers than having the patient sitting up and not moving.
The flatter the head of the bed, the better, because that takes pressure off of the sacrum, the most vulnerable spot. Unfortunately, that’s the absolute worst position for the lungs to expand. The more the patient is sitting up, the better their lung expansion. And blood pressure, what about that? Sitting up makes the blood pool in the legs prompting thrombosis, and away from the brain when the pressure is unstable. The first thing we do when the blood pressure tanks as a stopgap, is to lay the patient flat so they can continue to perfuse their brain. We’ll elevate the legs, too. ‘But wait, you said that laying the patient flat was bad for the lungs…’
You’re getting it.
It’s a constant game of robbing Peter to pay Paul. And that’s just one tiny aspect of critical care medicine. There are skills and nuances that take years, a career to acquire. So when the understandably uninformed public thinks it’s all about the number of ventilators, it’s dangerously short-sighted. You could have enough equipment to treat every patient, but who’s going to run it?
So going back to my lady, we laid her flat to turn her. NO ONE is getting turned every 2 hours in Covid-World, but we decided to try. We gave her small sedation and narcotic boluses, put on our PPE and went in. Upon the head of her bed being lowered, her SpO2 dropped to 79%. I could hold my breath until I turned blue, and probably couldn’t get it down to that before gasping for air.

She wouldn’t come back up. We turned up her FiO2 to 100% and suctioned her, but some of these patient’s lungs are full of infection, not mucous, and so far, there wasn’t much to suction. We called the PA and doctor and respiratory therapist (unsung champions) to the bedside and made adjustments to her breathing tube and obtained chest X-rays. We got blood gasses and changed ventilator settings. It took her forever to come back, and by the end of the shift, she was only up to 92%.
Basically, laying her flat de-recruited her alveoli. Her lungs collapsed, but on a microscopic level. The pressure settings were increased to re-inflate the little tiny grape-like clusters of minute air sacs.
Like I said, these patients are sick. Mouth care every 4 hours to prevent VAP- ventilator associated pneumonia? Apparently not that either. They can’t handle the stimulation. This patient’s blood pressure was hanging in a sweet spot on meticulously titrated doses of IV medication. And the clinicians quite frankly, can’t afford to spend so much time in the room due to the increased risk of contracting the virus due to prolonged exposure to increased viral loads.
Speaking of exposure, my N95 didn’t fit well. For one thing, I wasn’t fit tested. Fit testing is important. They have you wear the mask for a few minutes and then put on a clear hood. They squirt some aerosolized saccharine into the hood and have you move your head all around and speak. You absolutely should NOT smell anything. Well, I went into the bathroom and thought, wow, this bathroom is really clean! I can smell the bleach… uh oh…
Then, I went into an adjoining patient’s room to cover her with a warm blanket. She wasn’t intubated, so her room was full of Coronavirus in spite of the negative pressure. The patient smelled bad. Really bad. And I could smell it. Again, uh oh…
They gave me another type of N95. It worked better. I could still smell a little, but the straps were so tight they left marks and gave me a headache. I’ll still wear it on my next shift. It’ll hurt though. I’d rather be uncomfortable- massively-so, than catch this heinous disease.
The highlight of the day was unquestionably, the firefighter tribute. My preceptor urged me to go outside to the front entrance to witness it. A full battalion was parked outside, and all of the firefighters were there in their turnout gear. Four of them held flags- a full honor guard. The lights on the rigs were all flashing and they were working the sirens, “whoop WHOOP!” And then they started blasting music. I have always thought the Journey song, “Don’t Stop Believin’” was heinously cheesy, and have a private bad association with it. But not now. They blared it. And cheered. And the civilians cheered and clapped and held signs. And we cheered and danced and clapped for them.
And I took the worst video of the proceedings possible, because I was ugly-crying behind my eyewear and mask. I was overcome with regret that I hadn’t come sooner, when the need was so much more desperate. All I can hope for is to be of service to these clinicians to the best of my ability.
I don’t think a few weeks is going to be enough for me to feel in any way worthy of this level of tribute from New York’s finest. I just hope that my best is enough and to be useful. I guess it’s something for me to be part of the relief effort. If my presence means that another nurse has a lighter assignment by even one patient, that’ll have to be enough. By the way, the nurse orienting me said that the firefighters do this with different music, but the same enthusiasm, every single evening.
Sunday, 4/26/20
Not much to report today. Just feeling contemplative about everything. Last night was a really rough bedtime for Andre, missing me. He was crying and in utter heartbreaking despair. David cuddled him in the big bed while I sang to him, “Somewhere Over the Rainbow.”
He seems a lot better today, but it’s really hard to be apart from my baby and my husband. I always tell Andre that he and his daddy are the two halves of my heart. They are my heart, and I can only be away from them for so long. Three more weeks is an eternity, that hopefully, will go by quickly. I can’t write too much about it without getting depressed.
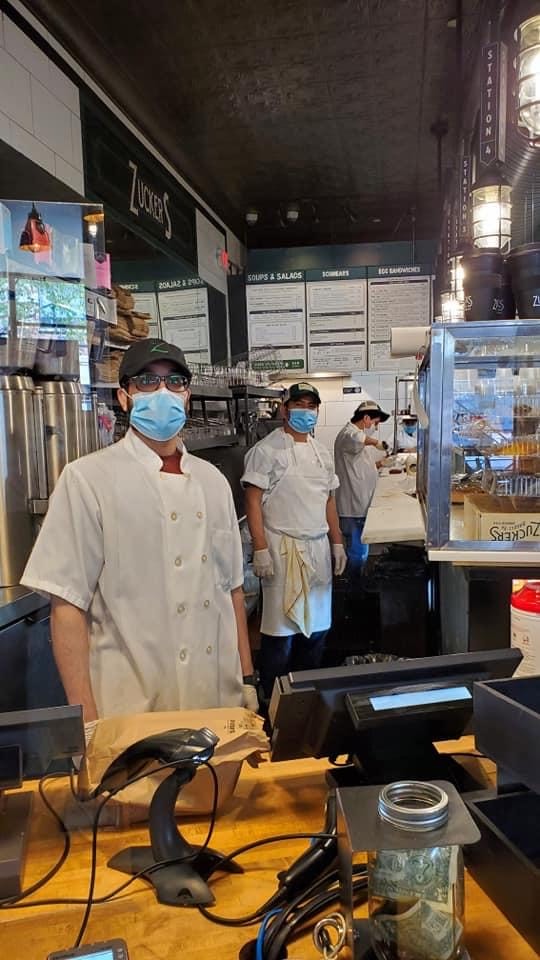
It was nice to do my laundry and go back to Zucker’s Bagels and Smoked Fish, where Chris (one of the guys who works there) remembered my name after just one visit. I guess I was goofy enough to make an impression. He called me, “Becky,” a moniker I loathe from just about anyone but my Philly firefighters. I told that to Chris, and that he can be a part of that select few.
Tomorrow I go back to the ICU, this time on my own. Heaven help me.

Monday, 4/27/20
Exhausted. So much I’m shaking. I’ve just forced myself to eat dinner- usually NOT one of my challenges.
I’m confused by this disease. My patient today was an 82 year old woman who fell down at home and hit her head, causing a brain bleed, luckily not a terrible one. She also has Covid-19. She has it in the way that I have blue eyes. It’s an incidental finding, asymptomatic, contagious for sure, but not to her detriment apparently. She’ll finish getting treated for her neurosurgical problem, and hopefully go on her merry way back home.
The patient in the room next door is my lady from Saturday. My age, with only one well-controlled comorbidity, she’s gotten far worse. She’s now chemically paralyzed in preparation for being pronated. Pronation is when a patient is positioned on their stomach, face down- face turned to the side actually, to maintain their intubated airway.
This is a last-ditch effort. There’s almost nowhere to go on the ventilator settings, and pronation allows the bottom and rear portions of the lungs to re-expand, and for any drainage that’s been just sitting there, to mobilize. They stay on their belly for 16 hours, and then get turned back over onto their back again. Arterial blood gasses are taken every 4 hours to evaluate how well it’s working.
The problem with Covid-19 and why it’s nothing like the flu, is that the flu can lead to pneumonia. Your lungs get junky, you get secretions. You either get over the viral part of it with time, or take antibiotics to combat the secondary bacterial component. Then, usually, you’re done.
Covid-19 is insidiously nasty in ways we’re just beginning to understand. With Covid-19, the lungs aren’t always full of secretions, they’re full of infection. And then there’s the micro-clots. The micro-clots can affect every system, including the brain, heart, lungs and kidneys.
There’s not just a temporary condition that resolves with time and treatment like with the flu; there’s damage. Often permanent debilitating damage. The kind that leads to pulmonary fibrosis- irreversible lung scarring, cardiac damage, impaired kidney function, and strokes. And because it’s brand new, no one really knows what the long-term effects are for the lucky survivors of critical Covid-19 infections.

Some are reporting that those who go home after these prolonged ICU stays aren’t quite right. It’s ugly, and it’s unfair, and there seems to be no rhyme or reason for who gets a mild case, and those for whom it’s fatal. I feel like I’m getting the education of a lifetime, and the nursing experience of a career, but at a terrible cost. They didn’t want to prone this lady initially. Because she’s so tolerant of the sedation- hard to fully sedate, they’ve been reticent to paralyze her. There’s probably no more horrifying predicament than to be paralyzed but alert and aware, and unable to communicate. It can lead to debilitating PTSD. But she’s going to die if they don’t, so they place her on some different sedation drugs and snow her with them.
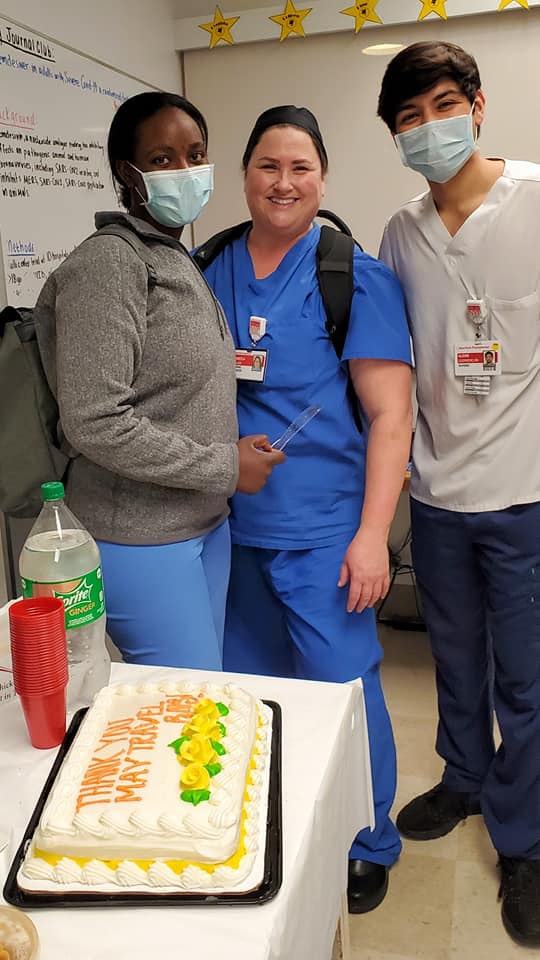
In spite of the sheer gravity of the situation, I’ve never had a more positive experience in my entire nursing career. The physical plant of the hospital may be old and run-down, but the culture is incredible. I’ve worked at my San Diego hospital for over ten years, and I’ve never met the Chief Nursing Officer. I wouldn’t even know her if I ran into her.
Today was my second day in the NYP ICU, and I met the CNO and COO. They stopped at our workstation and asked us about ourselves, where we were from, what brought us here, and how we were doing. They expressed their sincere appreciation.
The unit is overstaffed, but they’re not even thinking about cancelling travel contracts. They know their staff and round regularly, greeting them by name. They are the senior-most management, but their offices are, by choice, in the basement. This is because they want to be in touch with everyone, including the janitorial staff. I’ve never experienced this kind of leadership before. It starts with them and filters down to the middle and lower management.
Everyone is hugely supportive. These managers know what time of day it is on the ground, and they are committed to supporting their traumatized staff. They are consciously over-staffing because they know that their clinicians are shell-shocked and need a break. And the staff are magnificent. The cohesion is there, and they work together seamlessly. It would be easy to feel proprietary when overrun with temporary workers, but they are appreciative and welcoming. They are grateful for the help.
I’m scheduled to work on Mother’s Day. I won’t be able to celebrate with my own child, so I’m glad to enable at least one staff nurse to enjoy the day with her own. I continue to feel so incredibly humbled.
I hope my lady makes it through the night. Saturday she was following commands and interacting. That’s how quickly patients can take a turn for the worse. On Saturday I thought of her as “stably-unstable.” Now she’s just unstable. Her body is under attack, and I just hope to God she wins. I’ll find out tomorrow morning when I go back in. For tonight, I’m exhausted. And maybe a little proud of myself for performing well. That’s been my goal from the beginning. I feel like my fatigue is earned.
Tuesday, 4/28/20
Exhausted. Don’t feel like writing.
I recovered an ICU admit today, an RRT from the floor. The Rapid Response Team is called for various criteria outside the ICU- indicators that the patient is declining. It’s a precursor to calling a Code- an attempt to avoid a Code.
The criteria are usually: a sustained or unusually high (or low) heart rate, a dangerously-low (or high) blood pressure, a change in mental status, a decrease in blood oxygenation, a decreased urine output, and my favorite, the intuition of the nurse that something is wrong.
A nurse spends more time with the patients by far than the doctors. We know our patients, and that 6th sense should be honored. If it turns out that nothing is wrong particularly, the RRT is ideally seen as a teaching moment; no one is ever (or should ever) be chastised for calling one, as we don’t want floor nurses to ever hesitate to make that call.
The activation of an RRT goes above the immediate 1st Call resident, and calls to the bedside an attending physician, a respiratory therapist, and a critical care nurse. They ensure adequate IV access, obtain 12-lead EKGs, labs, and provide increased support at a higher skill level. Usually a transfer to the ICU ensues, and that critical care nurse stays with the patient until that happens.
My patient was found to be unresponsive with an SpO2 of 26%. To put that into perspective, a donut will usually have one of 50% or so, even if without a heartbeat. 26% is lower than an inanimate object- not even a reliable number. The patient has Covid-19, but they think he also may have aspirated. He has a feeding tube in the right place, but if he has an insufficient esophageal sphincter, some regurge isn’t unthinkable, however unlikely.
It’s likely to be a turn of his Covid-19, but he had (and has) a lot of secretions that do look suspiciously like tube feed, so aspiration is the going diagnosis. Still, secretions and coughing and Covid-19 are less than appealing conditions to go into, even in a negative pressure room, so I didn’t want to bring my helpers, two med-surg nurses into the room any more than I had to.
These young women are fantastic and have lightened my load considerably. One helped me to do an epic repositioning, cleaning, and linen change on the patient. It mobilized a ton of secretions so I could suction them, and mobilized other bodily processes as well. He was a tall guy, not huge, but not tiny. He was also incredibly stiff, so it was hard to turn him. I put my back into it more than I probably should have in order to spare hers. For the rest of the shift, I turned him myself, to further limit her exposures.
The patient who had been unresponsive previously, groaned through the big repositioning ordeal. We reassured him. At the end, he murmured his thanks. We asked if he felt more comfortable, and he said yes. It felt wonderful. This is why I do this. My gift to him is really his gift to me. I made a difference in his life. I gave him dignity and comfort. I’ve earned my carbon footprint for another day.
I ended up getting my N95 fit test, and passed without smelling the saccharine spray. Back in the ICU however, I can still smell the bleach, sanitizing wipes, poo and pee. Luckily, my colleagues assure me that so can they. I feel a little better about my protection.
At 7pm, I went down to the nightly firefighter tribute. This initial surge is declining. The tributes have to end sometime, and these will end on Thursday. It might be my last chance to see it and film it. I did so.

No music tonight, but instead they blared their sirens on full blast. I probably lost some hearing, but it was worth it. I took a picture with a firefighter named Frank. He gave me his number so I could send him the video. I ended up friending him on Facebook so he could see them all. He is the father of twins who are exactly the same age as Andre. His ladder company is directly across the street from the WTC.
How can he be applauding me? It’s ass-backwards. I try to explain that I’m just here for a few weeks to take some pressure off the REAL combat veterans, after the peak of the battle, no less. He’s not having it. He’s insistent on giving me my due, and I feel like a fraud.

I crawled home, my lower back protesting every step. I passed a really New Yorky pizza place, and even though I had food at the apartment, I bought a slice.
I ate it in the bathtub.
Wednesday, 4/29/20
I woke up early this morning. I’d taken ibuprophen, magnesium, and a muscle relaxant last night, so I slept hard. But when I started to get out of bed, my thigh cramped up like a rock, all the way around- inner, outer, front and back. I punched it with my fist in desperation. Finally I was able to get up and take more of the same as last night. I forced myself to drink a ton of water. Even though I’m trying to drink a lot of water, I think I’m dehydrated.
As the day’s worn on, I feel under the weather- foggy, scratchy throat. I have a tiny pulse oximeter with me. Some Covid-19 patients feel fine, but their SpO2 is in the 80’s and their chest X-rays look heinous. I chastised myself as I measured my blood oxygen. Normal, of course. I’d have to have been exposed on my first day to be symptomatic. I feel just as shitty after a hard shift and muscle relaxants at home. But of course, nothing is normal now.
I’ve spent the day watching TV and taking a nap, but at 6:30pm, I’d like to walk to work and experience one last firefighter tribute. I won’t go tomorrow night. That last tribute is for the core staff, as far as I’m concerned, and for them only. It would feel unseemly to attend.
Then again, maybe I won’t go tonight. I’m tired and a little down. I miss David and Andre. I miss my own, albeit less comfortable bed. I miss our cat, my friends, and my little island home. I want to feel those two precious pairs of arms around me and my arms around them. I want to hold that little body and breathe in his hair, kiss those chubby cheeks.
The local news is on TV. A hospital far away is having one of those happy celebratory discharges of a Covid-19 patient. She was on a ventilator for 2 weeks and is now going home.
Why is this making the news? Because it’s so goddamned rare. The public sees these encouraging feel-good stories and gets the wrong idea. Also on the news, the Department of Defense is dispatching mental health professionals to New York. Ones that specialize in combat stress.
I didn’t go to the hospital tonight. When I got downstairs, it was raining, and given that I don’t feel great, I decided to call it a day. Hopefully I’ll feel better tomorrow.
Thursday, 4/30/20
Again, too exhausted to write. So exhausted that when I got home, I tried to get into my next door neighbor’s apartment. I fiddled with the key, confounded as to why it wouldn’t turn in the damned lock, until the occupant banged on their side of the door, startling me out of my reverie. I stammered an apology and slunk to my own apartment. I slept well.
Friday, 5/1/20
Today was a good day. My lady is soldiering along, but she’s in for a lot of suffering no matter what her outcome.
From the beginning, she’s been a tank with regard to sedation. Although she has no history of drug or opioid use, she really requires a lot. On Saturday, with pretty significant amounts of sedation, she was responsive and following commands. Although she was on a ventilator, she was able to indicate that she was comfortable and didn’t need increased sedation. It was pretty interesting. Over the next day she declined, requiring more and more oxygen, and the decision was made to paralyze her and deepen her sedation so she could be pronated.
Even so, she still has managed to follow some commands, like opening her mouth for oral care, which is crazy. She’s on steroids to combat the inflammation. That causes her blood sugar to go sky high, necessitating epic amounts of insulin. She’s about 8 liters positive, and to diurese her at this stage would kill her.
We keep track of every drop of medication, water, and tube feed that goes in, and every drop of urine that comes out. She’s gotten 8 more liters of fluids in than she’s put out, and that means she is terrifically swollen. The swelling follows gravity, and she’s face-down for 16 hours out of 24, so it’s particularly pronounced in her neck and face. Her eyes are nearly swollen shut, and her poor lips are a Kardashian nightmare. Her tongue protrudes, because it’s too swollen to fit inside her mouth completely. We’ve started Benadryl today to help with that, but also, because she has a rash over much of her torso. This could be from the medication, or it could be from microclotting in her skin. We’re not sure.
She also has random blisters. We bathe her daily with antimicrobial solution and sprinkle her with antifungal powder, and cover the blisters with foam dressings. There are foam dressings on the front of her ankles, feet, knees, nipples, shoulders and clavicles, and sternum. These are to prevent pressure sores when she’s on her stomach.
She’s on a fentanyl IV drip. This is a narcotic for pain control, and she’s on a lot of it. A side effect is constipation, and possible impaction. She hasn’t had a bowel movement since I started taking care of her, which was 5 days ago. I really don’t know when she last had one. I approach the PA about the need to get more aggressive with her bowel regimen. The tube feed is going in, and it has to come out. Plus, any impaction in her belly will press up against her diaphragm and lungs. She has to poo.
We increase her stool softener and add 2 different laxatives and a suppository. I hope it will work. I tell the PA that although this will make my job a lot harder, it’s what the patient needs. She is prone when I start my shift, and at about 9am, we supinate her- or place her on her back. This requires at least 5 people. 3 are physical therapists. They have morphed into the pronation team. They do the lion’s share of the work. They know where to put the foam dressings, how to take off the EKG leads (they will be placed back on the patient’s chest), and how to sandwich the patient between sheets, paper chux, and a turning/sliding mat. I manage the arterial line, the multiple tubes going to the central line in her neck, the urinary catheter, and the peripheral IV’s. The respiratory therapist controls the breathing tube and makes sure that it never gets dislodged or occluded. Additionally, another ICU nurse stands outside the room with the IV pumps, prepared to bolus sedation if the patient stirs, or to run and get needed supplies.
In the afternoon, as we prepare to turn the patient back onto her stomach, I send the outside nurse to get a rectal tube. The bowel medication has worked, and the patient has had a bowel movement. I get to work cleaning her. The PT’s lift her legs and even the PA is helping to turn her. As I clean her, just as one would a baby, her reddened angry fragile skin sloughs off, tearing away no matter how gentle I try to be. I wince with contrition and apologize to her. I’m hurting her, but there’s not much I can do about it. I have to clean her. I cover her poor skin with a thick white barrier cream, and insert the rectal tube. It is held in place by a balloon that I inflate with water, that keeps it in the rectum. This is essential. Her skin can’t afford to be in contact with any more stool, and she can’t be easily cleaned on this turning schedule.
We continue to draw labs, make adjustments to the ventilator settings, and titrate medications. We will start her on Remdesivir tonight. It’s a clinical trial, and she meets the criteria. Her family has consented. I look it up to see if it needs to go through a central line, and if it’s compatible with other IV medications. There’s no information to be found, because it’s brand new. The PA gives me some guidance.
The PA’s are fantastic- knowledgeable, approachable, and available. I love working with them. As we do these turns, especially this last one, my goggles build up so much condensation from my sweat, I can barely see. I am soaked. After I take off my PPE and leave the room to wash, I am fatigued. I stuff my headband- designed for wicking away sweat with yoga, into my pocket. I can’t reuse it today, because it’s sopping wet. My scrubs are sticking to me. I sit.
And then the realization sinks in.
I’ve been busy with this patient all day, and I’m tired. One patient. A few weeks ago, these nurses were taking care of FOUR just like her simultaneously. No wonder they’re traumatized. To deliver the highest standard of care to this patient has kept me busy. How would I do it with four? Not well. Not to basic standards. Not to my standards, just like it undoubtedly wasn’t to theirs. How would I feel if I couldn’t give my lady the level of mouth care she needed, and had to leave her gargling on secretions because I had three others who each needed something more pressing to keep them alive?
I feel tired, but proud of the care I delivered today. How must they have felt, as their patients declined around them, deprived of everything but the sheer basics? How could they not break from the stress of just managing blood pressures and airways for that many, who could each, in a normal setting, be one-to-one assignments. They are traumatized, my NY colleagues. They did the best they could, a herculean effort, knowing that it wasn’t enough, and probably wondering how much better their patients might have fared had there been enough staff to really meet those patient’s needs. It’s heartbreaking.
This morning, I left a note for my neighbor, apologizing for the attempted break-in. I explained briefly my situation. This evening, I came home to an incredible card from him. He had written:
“Hello Rebecca,
Thank you for your note, you don’t have to apologize. I should say thank you to you for your dedication and coming to New York to help us.
I found you a quote which I hope you will keep in mind every day. It says…
‘“Helping one person might not change with world, but it could change the world for one person.”’
-Anonymous
My one exception to this quote is that I believe in your case and in the case of all your colleagues, you ARE changing the world. In fact, you’re saving it and you’re saving lives, so thank you!
Please be well, stay safe, stay strong, keep your spirits up, and may God bless you always!
-Ed”
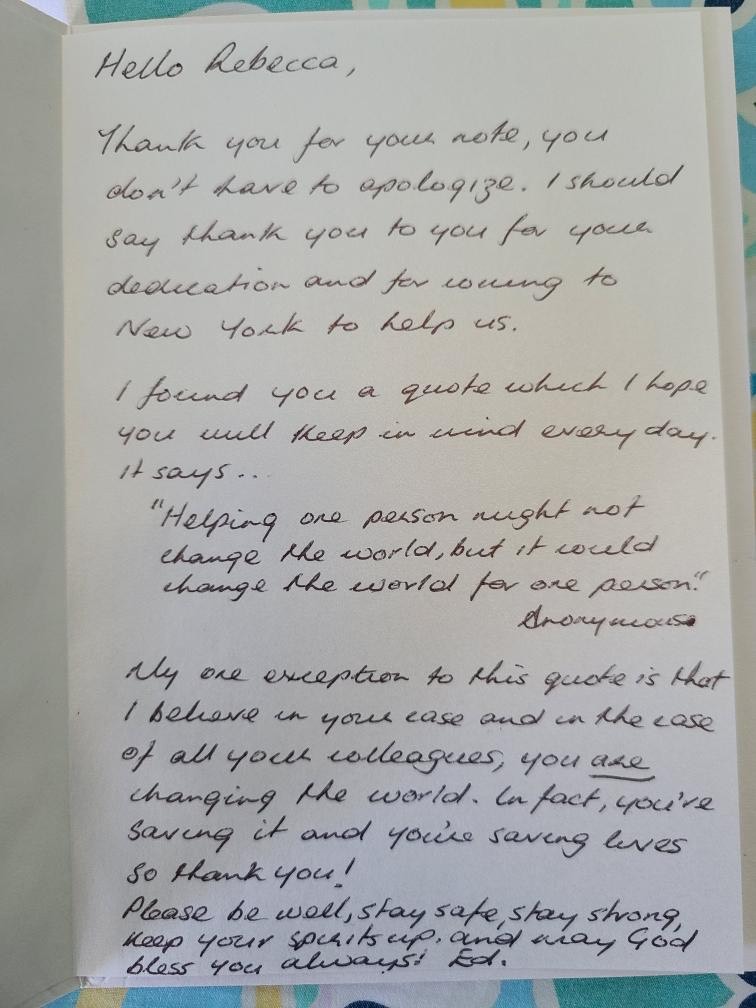
I’m so moved. His words were beautiful. A stranger, but with so much caring. I am stunned by the beauty I’ve discovered on this trip.
Saturday, 5/2/20
I usually don’t write in the morning, but it’s such a gorgeous one today. It’s sunny with blue skies, balmy, and I’m OFF today!
I’m doing laundry, but when I’m done, I’m going to go try and pick something up for Frank’s firehouse and drop by for a visit. I just shot him a text to see if his platoon is working this weekend. The Philadelphia Fire Department goes on a platoon schedule, A, B, C, and D. They alternate from 10 hour day shifts to 14 hour night shifts, 2 days, 2 nights, and then 4 off. Not sure if NYFD does the same thing.
In San Diego, all firefighters are paramedics, but the east coast is different. The roles are more delineated. The old school firefighters hated being forced to be EMT’s. Those guys are probably all retired now. It’s been 25 years since I was a paramedic and steeped myself in that culture, and I imagine a lot has changed.
I’m still blown away by the card I received from my neighbor. I was prepared for a heinous clinical experience here in New York, but I was completely unprepared for the human component. The people. I’m staggered by the warmth, compassion, and frankly, the love I’ve encountered here.
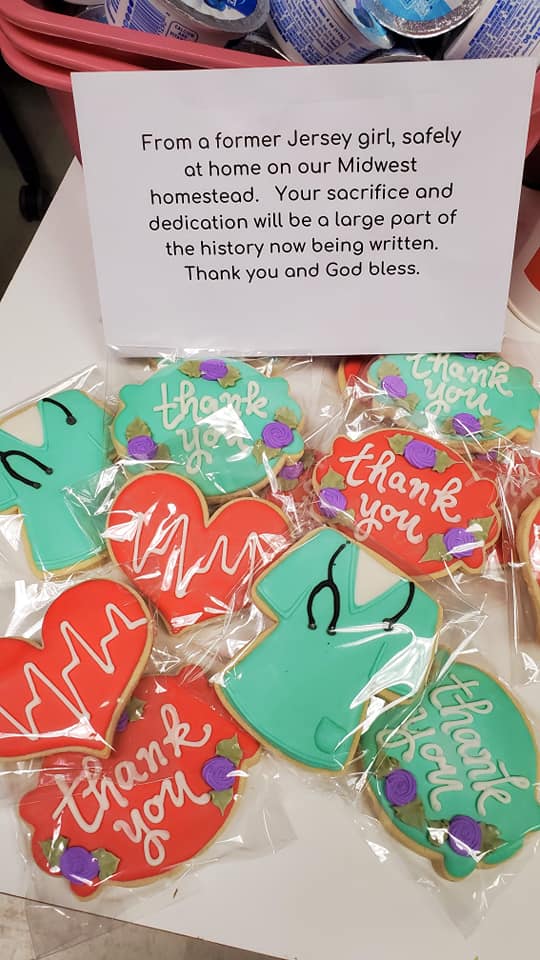
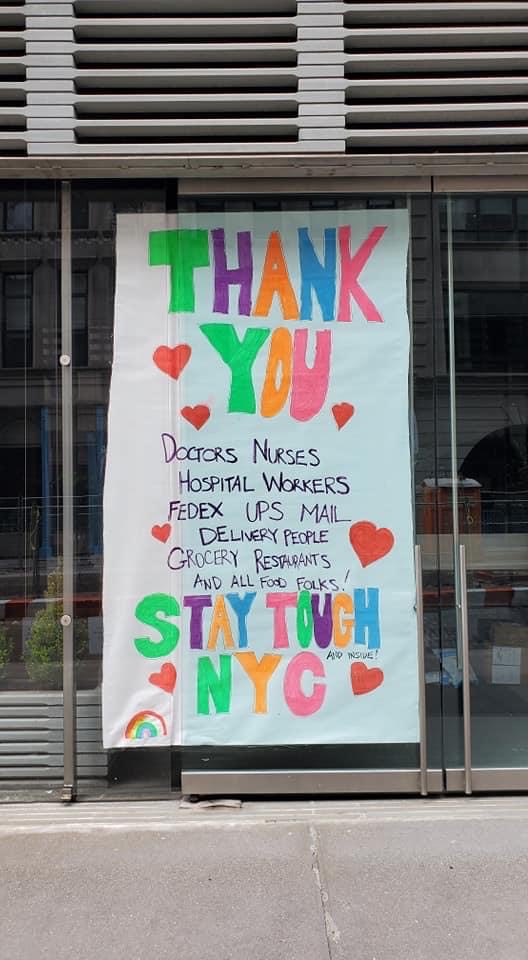
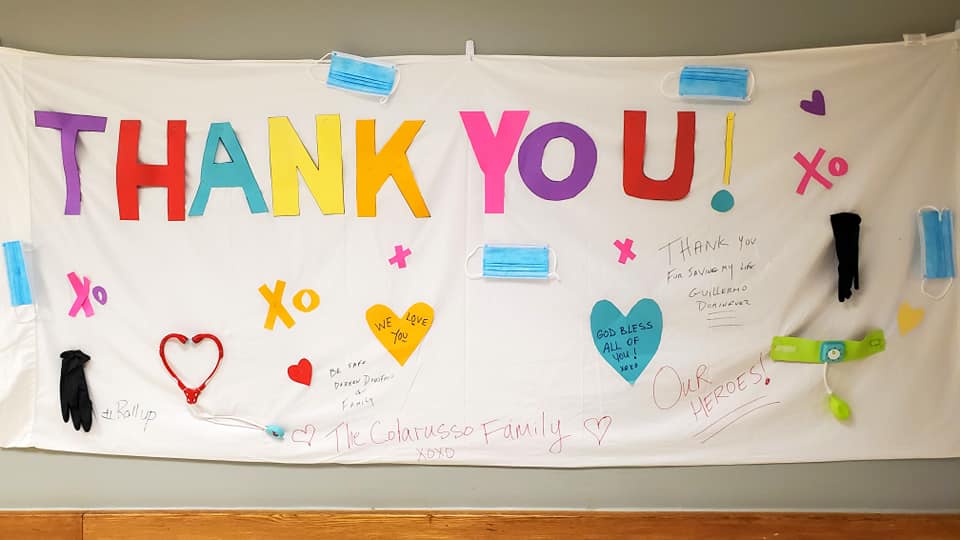
The strangers who make noises of every kind for the frontline workers every night at 7pm. The guy who goes up to the rooftop garden to howl his gratitude. The pregnant couple who brought their 3 year old up to the rooftop to beat his little drum. The nice guys at the bagel shop and the pizza shop. The man on the street last night who shouted, “Thank you!” to me from across the intersection as he saw me walking home in my scrubs, and the ladies with the dogs who did the same. The doormen of my building who knew my name within moments of arriving and never forgot it, buzzing the door open for me the moment they see my approach. The endless battalions of firefighters who alternated in giving tributes, probably not only to my hospital, but all the others. The neighbors of the hospital who showed up along with the firefighters, holding homemade signs and waving madly at us. The nurses, PA’s and doctors who welcomed the travelers with open arms and appreciation.
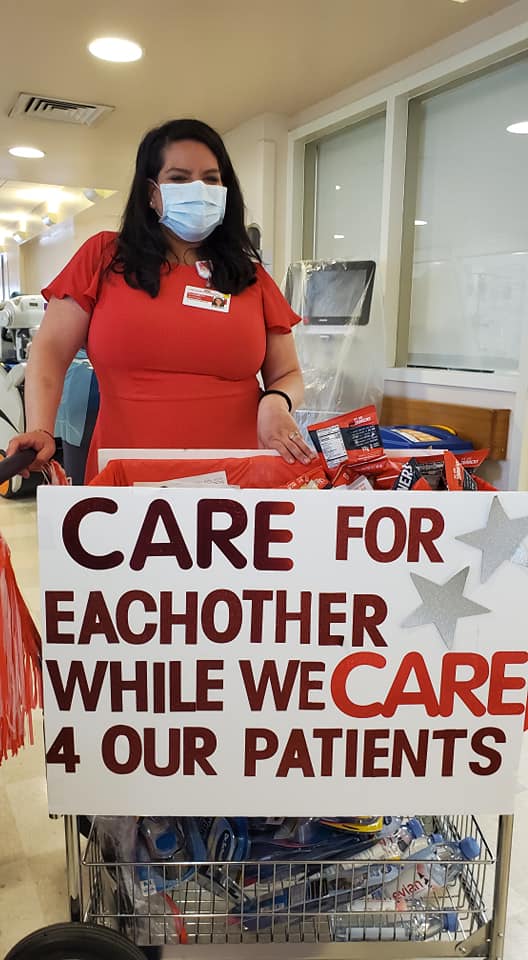
The management, who assured us that no matter how low the numbers fall, they will not cancel contracts. Those same managers who brought us all in to relieve their traumatized staff, and have taken the time to get to know us, from the CNO down to the assistant manager, endlessly supportive of their staff. Those same managers who have supplied the clinical staff with 3 meals a day, endless snacks, and water, ensuring that I will not, unfortunately, lose weight on this assignment. The unit clerk who offered me different N95’s until I could find the best one, and encouraged me to change it when it got soaked with sweat and condensation and stretched out of shape.
The other travelers, who are also supportive of each other as well as the staff. And the long-distance support from Coronado. People who want to help document my experience, strangers who inquire about my well-being and want to send me a care package. The small handful of colleagues who have reached out to check in and support me.
I expected to get battered, but instead I’ve found only warmth, appreciation, gratitude, and support. It’s mind-blowing, and amazing, and life-changing. It’s something that I can never forget.
Well, I took my walk. It is 73 degrees out, and although nothing has reopened, NYC has awakened to greet the Spring. I regret not bringing my flip flops. The chilly grey ghost town that first greeted me is asleep no longer, and it’s a huge change from 2 weeks ago. The trees that were budding and flowering are now gently leafing out. The tulip beds that surround some of the trees and parks are losing their petals and beginning to wilt.
The nearly silent streets have more vehicular traffic, and the locals are out on bikes and on foot. Teenagers and young adults rattled by me on skateboards, and I actually had to wait a minute or two before I could cross my neighborhood bike path, so many bikes were zipping by.
I went to the site of the WTC memorial at Ground Zero. It was roped off, the fountains were off, and the museum was closed, but I could still get very close- close enough to read the names engraved along the edges. Someone had stuck a couple of white roses in the grooves of the names. To actually see it in person was sobering, and I’m sorry I won’t be able to go into the museum on this trip.
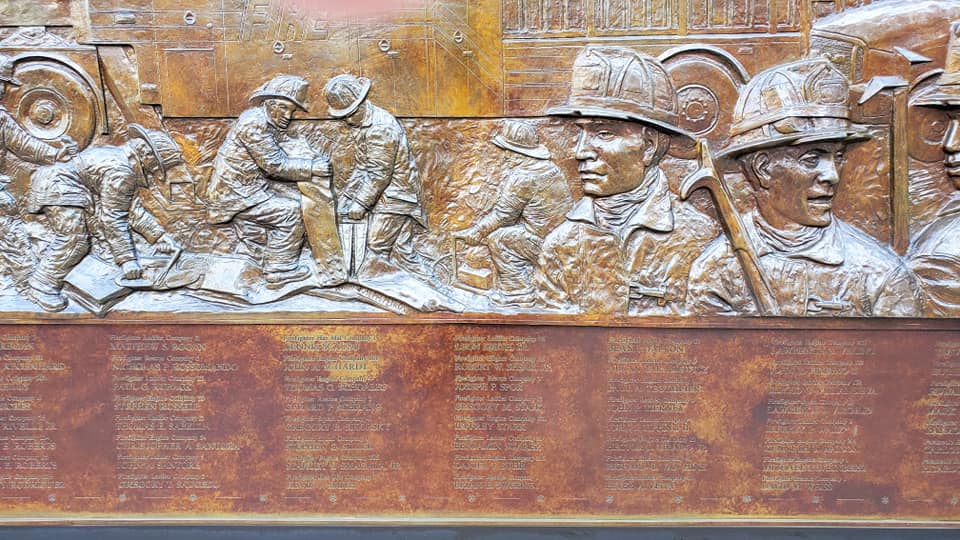
Across the street, as Frank had said, was his firehouse, Ladder 10. Right there, at Ground Zero. Affixed to the outside of the station is the 911 Firefighter Memorial Wall.
A huge bronze relief, approximately 5 feet high and 50 feet long, depicts the tragedy. The towers are in flames and billowing smoke in the center, and on either side are scenes depicted of first responders attending the disaster. On the bottom, stretching the full length are the names of the hundreds of firefighters who perished, including their officers and a chaplain. A couple of the guys were standing outside and I chatted them up for a minute or two, thanking them for their wonderful tributes at the hospital. When I explained that I had missed the worst of the surge and was just visiting to provide some support, one said to me, “we’re all in this together.”

And so we are. As I write, the 7pm salute is louder than ever. It’s as if the Yankees have won the pennant. I hear someone yell, “We love you!” I yell back, “I’m a nurse, and I love you, too!” And I do.
WEEK 3
Sunday, 5/3/20
I chilled out most of the day, and then took a long walk in Battery Park, along the Hudson to the southern tip of lower Manhattan. Flowers were in bloom, the trees in freshly unfurled new leaves, and the water was lapping along the edge of the waterfront.
A ton of people were out, with no evidence of social distancing. Only about half were wearing masks, and of those, only about half were wearing them correctly- over nose and mouth. When 7pm rolled around and people started cheering, I felt irritated. I wanted to carry a sign proclaiming, “If you’re not going to wear a mask, don’t bother cheering for healthcare workers.” I tried not to let it get to me too much. It was nice to see the Statue of Liberty, the Staten Island Ferry, and an NYPD fireboat chugging along.

Tomorrow begins my third week at NYP. I have no reason to feel nervous, but for some strange reason, I feel a sense of unease. Maybe seeing all of the New Yorkers flaunting social distancing took some of the shine off the Big Apple. I still love it here, and am still very glad to be helping, but I miss David and Andre and my more familiar life. It’s a honeymoon period here right now. Everyone loves and supports everyone… for now. I don’t know what the future will bring, either immediately or in the longer term.
I firmly believe that my time here is in the trough between the first and second Covid-19 wave. I also worry that the next wave will hit soon, and hit hard. It did in 1918, and there’s no reason why this should be any different. If today’s observations are any portent, the warmer the weather and the more the city opens up, the more this virus is going to spread like a pinball machine.
The city/the country/the world can’t remain in lockdown indefinitely, but people need to realize that when it all opens back up, we’re in for some real pain. I’ll be sorry to be unable to come back here to help with the next surge. I’ve promised Andre that I won’t do this again. My bosses wouldn’t let me if I wanted to.
A large handful of nurses came in sort of a delegation from their hospital in Utah. What’s wrong with the culture of my hospital that it doesn’t have the humanity and generosity of spirit to support the same? I’m tied to my hospital with what we refer to as “the golden handcuffs.” The benefits, pension, and pay, as well as the security of being protected by a strong union, are too good to leave. The fact that we NEED a union to protect us however, is demoralizing. It is an institution that sees us as expendable and easily replaceable. It’s all about numbers and revenue. I’m comfortable there, but I don’t exactly feel supported. Maybe that’s too high an expectation of an employer, but after seeing how they do things here, it’s a little depressing.
Anyway, it’s the second eyewall that really does the damage in a hurricane, and I think that when it hits with this virus, it’s going to knock the world on its ass. I’m sure I’ll have plenty to do in San Diego.
Wednesday, 5/6/20
I skipped 2 days of entries. Because I was bloody wiped out.
On Monday, my lady got extubated. We lightened her sedation and watched her get more and more restless and agitated. We tried to reorient her, reassure her, explain everything to her, but even though she was with it enough to follow commands, she was just panicky and impulsive.
We explained to her that we needed to try her on a different ventilator setting for an hour (it had been only 10 minutes) to make sure she was able to really breathe on her own. She insisted, indicating “Now! Now!” while banging her arms and kicking her legs and glaring at us, to the point where the PA said “just do it.” We expected her to calm right down when the tube came out, but nope. She continued to be incessantly restless and irritable.
We still had her maxed out on Precidex, a continuous IV sedation drug that doesn’t affect the respiratory drive. I’d be obtunded on it, but she, as I’ve mentioned, is practically untouched by sedation. I continued to try and reorient her, providing emotional support and holding her hand, trying to explain that she had tubes in her bladder, rectum, internal jugular vein and the radial artery (in the wrist). Not to mention all of the monitoring wires to her chest, finger and arm. She wasn’t having any of it. I secured her lines as best I could and alternated with restraints on/off for the rest of the shift, sometimes having to don my PPE as fast as I possibly could to run in and try to get her to chill the hell out.
There’s a phenomenon called ICU delirium, where after long stays and tons of drugs, these patients lose all sense of a circadian rhythm. Day and night get reversed, and they hallucinate. This wasn’t it. At least not completely. She knew who she was and could tell me she was in the hospital. She could follow commands in the moment, but just couldn’t sit still for a second. I asked her to. “Please,” I begged, “I need you to NOT move for 5 seconds while I untangle this,” and she wouldn’t make it past 1. So I went home exhausted. Too tired to write.
Yesterday was worse. She was oriented completely, but just as restless. We titrated her sedation off, gave her Haldol (an antipsychotic) and Ativan (an anxiolytic), but they didn’t touch her any more than they did the day before. Ditto with the Benadryl. She was oriented now to everything, but her behavior was, simply put, crazy. We wondered if she had some sort of pre-existing psychiatric component to her alarming level of restlessness, impulsivity, and neediness. She simply couldn’t lay still.
I went in COUNTLESS times to reposition her, change and straighten her linens, and make sure she was snug as a baby. And like a toddler in a temper tantrum, she would roll and wiggle and scoot around until her lines were tangled or coming off, and her pillows were on the floor, and then she’d bang against the side of the bed for me to come in and pick them up. She wanted her cellphone. I gave it to her. She wanted her glasses. I gave them to her. She wanted the call bell, insisting I’d lied to her and never gave it to her, although I could produce it from the disheveled linens right next to her.
She alternated between telling me I was treating her like an animal, and apologizing. She said, in a rare moment of lucidity, that I’d saved her life because I was such a good nurse. I teared up and said it was because she was so strong, and she cried. She said that when she was out of the hospital, she would come back and stand outside the hospital to thank me. I explained that I had come all the way from San Diego to take care of her, and that I wouldn’t be here for that moment. I promised to visit her in her new room when she left the ICU. We held hands.
We had our tender moment, and then she proceeded to make my life a living hell for the endless hours until the end of my shift. I removed as much stuff from her as I could. The restraints had been discontinued at 2am that morning. I removed the arterial blood pressure line from her radial artery. Her blood pressure had been stable for a while and she no longer needed frequent blood work, and she was going to rip it out and spray blood all over the room eventually, no matter how much I shellacked it down with tape. I removed the rectal tube, opening the door for her to roll around in her bowel movements. Thank God, I was inserting an IV next door for a colleague when she did just that, and my colleague dealt with it admirably. I could have kissed her for taking it on, and she, a former psych nurse, said, “no problem, I appreciate you getting that IV.”
At one point my lady was on all fours in the bed, reaching over the side rail looking for her call bell so she could use it a few hundred more times. It was in the bed next to her. I pointed this out as I ran in to make sure she wouldn’t fall out of the bed. “You treat me like animal,” she retorted.
The attending opined that she may well be encephalopathic. Covid-19 causes microclots, and her brain is probably showered with them. She’s being anticoagulated with medication, but who knows if it will help. She’s making a lot more sense than the day she was extubated, but that moment of love between us, the one where I left the room elated with her progress and feeling like all my work was worth it and that she is truly one of the few success stories, was long gone.
I felt abused, taken advantage of. We’d all explained to her multiple times that because of her Covid-19, we cannot go in the room every 5 minutes because each time is an exposure. She couldn’t be reasoned with. She could talk on the phone and text, and answer every question appropriately, but her behavior was anything but, as she pulled her gown up to her waist, legs spread, not a care in the world, continuing to bang on the bedrail every other minute for me to attend to something else of a non-urgent nature. I couldn’t get into the room quickly enough to pour her more water, so she spilled it all over the tray table. That kind of thing.
I went home with my back threatening to spasm, and feeling dejected, bordering on depressed. I’d left my family and traveled 3000 miles to care for her, straining my back and risking my life to care for this woman, and was run ragged by her with almost no indication of appreciation (she said “thank you,” just a few times, but never “please,” when demanding that I do whatever she commanded).
Here was one of the biggest success stories of the ICU, and I couldn’t even revel in it or take joy from it, because my resentment was so deep. I had to force myself to think “Covid encephalopathy” over and over and over, because by the end, I hated her, and felt enormously guilty for THAT. At the end of the shift, I had one of the helper nurses go in to do the honors when she had a bowel movement. If I’d had to do it just one more time, I would have started crying from what’s known as “compassion-fatigue.”
That’s where I was. Over it. I simply couldn’t even look at her at the end. I hid behind my computer for the last 15 minutes of my shift, watching her surreptitiously while she restlessly undid the helper’s hard work in moments. I gave my apologetic report to the night shift RN, and she took it in stride.
I limped home and focused all of my energy on being careful to not slip in the shower, I was so tired. I was in bed by 9:30 and asleep when David called me to wish Andre a good night. I’d asked him to. I’d rather be awakened than not tuck Andre in, and I did so however sleepily.
And now it’s a new day. It’s back to being grey and chilly. I bought cookies on my way home- 8 packages of Pepperidge Farms to bring to Frank and the rest of the firefighters. The firehouses are all closed to the public, but Frank laughed and said he’s been on the job longer than almost anyone, and he’ll give me a tour. It’s probably the most historically-significant firehouse in the world, so I’m looking forward to it. I know that seeing these guys may make some tears fall, but they’ll understand, and I’ll feel better for it. I’m going to get ready and go, but at this moment, I just want to go HOME.
One highlight of the week, was when I FaceTimed with Andre while at work. My colleague- she of the psych-nurse background, was sitting next to me, so she overheard it all. I’d wanted to send gifts to Andre from New York, to lighten his mood. Unfortunately, everything was closed. I decided to Amazon him a present, since he wouldn’t know the difference. I settled on getting him a stuffy, and picked out a squirrel holding an acorn. It was a terrific one with lots of detail, and reminded me of all the squirrels in the Manhattan parks. So when we FaceTimed, he held it up to show me, and I asked him what he’d decided to name it.

Andre said, “I named him ‘Nut!’ I wanted to name him, ‘Nut-S-A-C-K,’ but Daddy said it was a bad word.” I just shook with laughter, unable to speak, while Andre looked at me quizzically and my colleague guffawed next to me. Since Daddy had refused to explain what it meant, I took it on, while my colleague giggled away.
Andre was delighted to have potentially named his squirrel, “Scrotum,” and then we had to have that discussion when he started to run with it.
All’s well that ends well, I guess…
Thursday, 5/7/20
I never made it to the firehouse yesterday. The weather was cold and rainy and poopy, and my mood matched. I just stayed in. Also depressing, was the almost complete lack of support from my hospital and unit at home. One of our nurse educators wrote a beautiful email, with pictures I’d sent her, and sent it to the whole department. Almost no one responded.
Compared with the love and appreciation and support I’ve witnessed and experienced here at NYP, it’s bloody depressing. I know that the managers at NYP MUST care about the bottom line, but so far, it’s never shown. Just unparalleled generosity, much appreciated by the staff. I haven’t witnessed an IOTA of gossip here amongst colleagues. Only cohesiveness and support.
The only bit of negativity I’ve seen is that geared toward a certain physician. He talks to the staff as if they are his minions, and idiots who just fell off the turnip truck yesterday. When we extubated my first patient, I told a colleague, “I’m so excited! We extubated Ms. Doe this morning!” He piped up from behind me, “I extubated her. The respiratory therapist was just my arms.”
I could have vomited in my mouth. He’s really the lord of the manor. He’ll tell people in the break room, who are actively eating and drinking, to put their mask back up, and five minutes later he’ll bop into a Covid room sans PPE as if it’s the ten-second rule. Other than him, it’s Shangri-La here.
Today was better. My lady went to the med-surg floor. She was apparently a lot more appropriate yesterday, so they were okay sending her upstairs. I had two new Chinese ladies. Many of the patients, maybe most are Chinese, since Chinatown is very close. One of my new ladies was very stable and lovely. I transferred her out.
The other new lady is very sick, and had to be chemically paralyzed and pronated. We’ll see how she does.
Two patients died today on the unit and many are horrendously sick. I’ll write more tomorrow.
Saturday, 5/9/20
Yesterday was more of the same. Same patient, but once we supinated her in the morning, she was a little better, so we didn’t have to pronate her in the evening. She’s still sick as a dog though.
Overall, the ICU is fairly divided between patients who are crashing and burning, and those who are limping along and getting incrementally better, however slowly. It’s sad to see someone trached and vented who’s sitting up and completely lucid, and dying to talk, but can’t. Bored out of their gourd and missing their loved ones. I didn’t get a chance to visit my initial patient on the floor, but I will.
More pressing is Andre. He’s breaking down now every night, crying pitifully for me to come home now. My heart is breaking, and I looked to see if Jetblue can get me on an earlier flight, but they can’t. It’s killing me to be a source of pain for him.
I felt great about being here three weeks ago, because I was sorely needed. Now, I’m needed at home, and that’s where I want to be. The ratios have improved dramatically here, and they don’t need me like they did. I want to buy him something to tide him over, but I don’t know what. Something for him to get excited about. I asked him what he wants, but he can’t think of anything either. He wants me, and that’s the one thing I can’t give him for a week.
And now I have a cold. I hope.
Sunday, 5/10/20- Mother’s Day
Today was a good day. I worked.
I was assigned to an empty room for the first admit, but none came. I just helped out. I put a large-bore IV into a thrashing alcohol-withdrawl patient, helped with the tanking blood pressure of another, and tried to just be helpful in general. I started my day in the ED. I still felt under the weather, and although I wasn’t really concerned about Covid, I still thought it would be the ethical thing to do to get rapid-tested. 2 hours later they confirmed that I’m negative. Like I said, I wasn’t particularly worried, but it was nice to get the confirmation.
It was Mother’s Day, and of course this jewel of a hospital supplied each unit with several dozen loose roses of all colors in a big vat of water. We put them in urinals all over the unit.
The best part of the day was going up to the med-surg unit to visit my original patient, the lady we extubated who drove me bonkers. It was awesome. She was normal, not on any oxygen, and remembered a LOT. She even remembered that I was from San Diego. I brought her one of the roses, and we both got a little emotional.We FaceTimed with her mother who was elderly and didn’t speak English, but kept tearfully thanking me over and over. I told them both that it was her strength that had saved her life as much as my nursing, and I was really overjoyed.
This patient is really one of the few success stories of this pandemic, and it’s amazing that I had the opportunity and privilege to play such a key role. I was excited about it for the rest of the shift.
The hospital inundated us with food and treats from great restaurants, and I practically rolled home. Upon arriving home at my building, I was greeted with a vase of beautiful flowers from David and Andre, and a wonderful little package from some UCSD healthcare workers I’ve never even met. A PA and some nurses at the infusion center. The PA just knows me through a mutual acquaintance. It had a whole bunch of little niceties.

All in all, a really good day. Only six more days until I’m reunited with the two halves of my heart in Coronado. I can’t wait. I really will miss all of these special people here. I’m guessing it will all seem like a dream when I’m back at home.
Monday, 5/11/20
It was another very good day at work.
I cared for a very sick older Chinese woman. Unlike my lucky lady, this one probably won’t make it. She’s been in our hospital for over a month, has a tracheostomy, and is almost unresponsive on zero sedation. She was on CRRT, Continual Renal Replacement Therapy for weeks. It’s an extremely slow continuous form of dialysis. These patients are way too unstable to tolerate substantial fluid shifts.
She underwent regular hemodialysis in the morning, and it was touchy. She’s swollen. Her flesh resembles that of an overripe tomato. It’s scary to handle these patients because you’re always afraid their skin will tear. Although she has a ton of extra fluid in her body that’s causing all that swelling, she’s actually intravascularly depleted. There’s not enough fluid inside her blood vessels to maintain her blood pressure; it’s all leaking outside the vessels into her flesh, known as “third spacing.”
I have the dialysis nurse stop pulling off fluid, and put the head of the bed down, first pausing her tube feedings so she won’t aspirate. Her legs are already elevated. I ask the PA to order 25% albumin. Albumin is the white part of the egg- pure protein. When a concentrated form is infused, the protein pulls the fluid back into the blood vessels. It doesn’t last all that long, but it buys her body some time to adjust to the loss of fluid from the hemodialysis. She’s supposed to have 1.5 liters removed, but we hold at 1. She’s bleeding from somewhere. I’m suctioning blood from deep in the back of her throat. She’s had multiple bowel movements. I suggest testing them for blood.
We do, and it’s positive. She’s been anticoagulated with Heparin- a common blood thinner. Covid-19 causes all kinds of micro-clotting problems. Although she’s been off the Heparin for a day or so, she’s still losing blood. We gave her a unit this morning, and we keep monitoring her blood count. We’re also adjusting the ventilator constantly. Whenever we do, her blood pressure drops and we do that dance.
I’m careful drawing labs from her arterial line. This hospital doesn’t have a certain bloodless device that we have in San Diego, so I draw the waste blood into a syringe, instead of a tube to be thrown away, and once I get my samples, I reinject the waste blood back into her artery. She needs a ton of labs, and she can’t afford any more blood loss than necessary.
After her 3rd bowel movement of the day, I insert a rectal tube. I still find a little time to put a good IV into the hand of my next door colleague’s patient. She couldn’t find a vein, but I employ an old trick of packing the patient’s arm in hot packs and a blanket. After 15 minutes, I go back in and there’s my vein. I love putting in IV’s. Each one is a little challenge, and a little victory. It’s a big IV, so the nurse can get blood samples from it and give whatever meds she wants.
It feels good to help a colleague and we rely completely on team work. I helped get that same patient from a chair back to the bed with a special lifting device, and cleaned her poop. The nurse appreciated it, just like I appreciated having another colleague’s help cleaning up my patient’s three ‘Code Browns’. It’s all hands on deck, and because of that, things run smoothly and with good morale.
The patient looks a smidge better when I hand her back to the night shift nurse who gave her to me in the morning. Her CVP (Central Veinous Pressure) is better than before the albumin, which means there’s more fluid in her blood vessels, which means that her blood pressure is better. The rectal tube makes things better for the patient’s skin, and far easier for the next nurse to take care of her. The patient is relatively stable, and the room is clean and neat, and I go home to my apartment. Tired, but feeling good.
Tuesday, 5/12/20
A quiet day off today. Still feeling under the weather with a headache, malaise, and some congestion. I’m taking my vitamins, trying to drink water, and otherwise just chilling at home. Some laundry and a nap and TV. Of course I’m FaceTiming a lot with David and Andre. I’m just counting down the days now! I’m glad I tested negative for Covid, because I feel cruddy.
Wednesday, 5/13/20
Another good day at work. I took care of a pretty special patient- another success story.
This woman was a tiny bit older than me. She’s been in the ICU for about 7 weeks, and she’s been through the wringer. She’s been vented, pronated and on CRRT, and today, I sent her upstairs to med-surg. A sweet woman with a psych and drug history, she looks bad on paper, but in spite of her being incontinent of stool and urine every single hour of my shift, including when she was out of bed in a chair, and it all went on the floor, it really was a pleasure taking care of her.
People- the general public, have absolutely NO idea how much the words, “please” and “thank you” can make a difference. A little simple civility and appreciation goes a LONG way. She was physically and mentally exhausted from such a lengthy and heinous ordeal, but managed to still be appreciative.
She was embarrassed and apologetic about me having to constantly clean her up, and half of my nursing care was giving her the emotional and psychological support she needed. I’d tell her what a rock star she was, how proud we all are of her, and I’d blow her kisses from outside the doorway. Her face would light up. Her poor face, with a huge deep pressure ulcer on one cheek from the endotracheal tube holder while prone and face down.
When I got to the unit almost 4 weeks ago, the unit was over-full, and she was in one of the double-occupied single rooms. She looked none too good then, and it’s kind of amazing to see her moving forward today.
Many others still aren’t. We had 2 deaths on the unit today, and a couple of others are circling the drain. One was a DNR, do not resuscitate. The other was a long long code.
As I’ve said, this is virus is no joke.


In other news, I’m going back WAY fatter. They’ve been feeding us constantly. Every morning, croissants, danishes, and fresh fruit cups, as well as yogurt and breakfast bars. Lunch has been anything from salads to sandwiches, to killer pizza, lasagna, and the other day, chicken piccata. A few days before that, it was pasta with pesto or bolognaise. Dinners have been taco bowls, Caesar salads, and on, and on, and on. There’s just tons of food, and the majority of it comes from terrific vendors- local restaurants.
On days off, there’s GrubHub for better Chinese food than we have in San Diego by a long shot. With the city closed, chilly, and with me being tired from work, there hasn’t been a whole hell of a lot to do other than watch TV and eat. So, I’m fatter.
I also haven’t been feeling all that well- like a cold at low ebb for a while. There have also been a few concerning “change-of-life” symptoms that have been dragging me down, that I’ll refrain from elaborating on. The weight gain probably isn’t helping. Hopefully I can get my shit together when I get home.
Thursday, 5/14/20
Three more days. One more day of work tomorrow. At this point, I’m so ready. NYC has a thousand fabulous things to do in a normal world, but during lockdown, it’s just me working and eating and watching TV and going out for the occasional walk. I just want to be home.

Friday, 5/15/20
My bittersweet last day at work. I had my first non-Covid patient, a 29 year-old guy who’s alcoholism is so severe, he’s about to lose his liver. Giant distended belly full of ascites (fluid) and covered in visible blood vessels, skin mustard-yellow with jaundice, and hallucinating and disoriented from hepatic encephalopathy. Basically, his ammonia levels are so high, he’s pickled his brain, along with his liver.
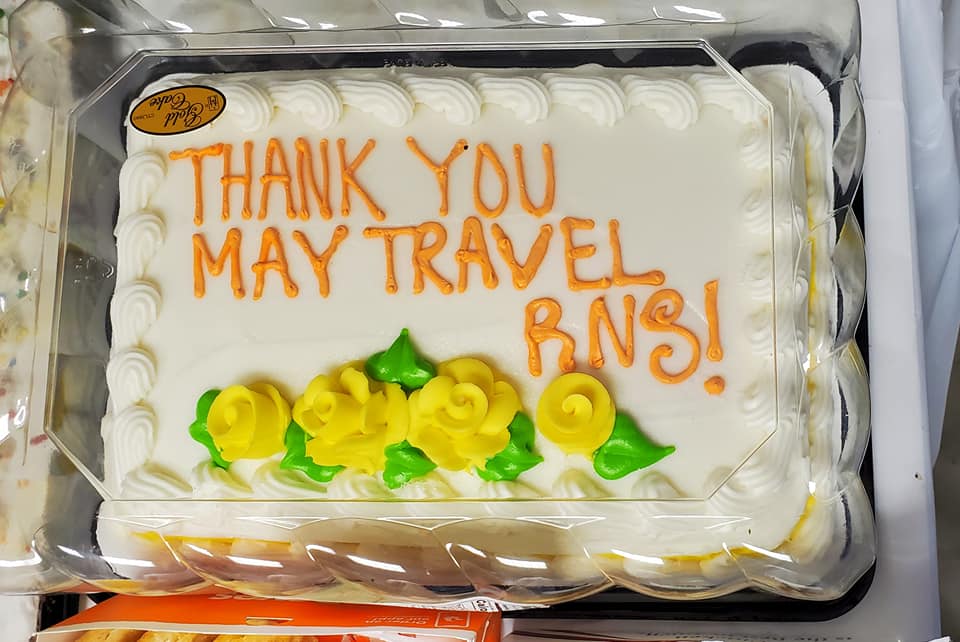
He was a handful. 29 and has drunk himself almost to death. Aside from that, it was a good day overall. My colleagues threw me and a couple of other travelers a party, gave us each a fleece blanket with the NYP logo, and that was that.
While still at work, I wrote the following letter:
Friday, May 15, 2020
Dear Esteen, Joan and Juan,
I am writing to you in a quiet moment here on the unit, on my last day of my 4-week contract. I haven’t been shy in voicing how impressed I have been with my experience here at NYP of Lower Manhattan, and as promised, I’m putting it in writing.
I am based in San Diego at a large university hospital in the PACU. As the surge in New York was reaching its peak, I, like so many across the country was riveted. I was marinating in the news and in Facebook groups devoted to Covid-19 healthcare professionals. My hospital, anticipating our own surge, began cutting way back on elective surgeries. As the days wore on, things got less busy, and people were increasingly urged to flex. I began to get more and more antsy, feeling like I wasn’t needed in San Diego where the surge seemed to never come, but WAS needed by my brothers and sisters in New York City, where the horrors were apparent. I’d heard about crazy ratios, running out of medications and equipment on top of sketchy PPE. I heard and read accounts of nurses being run ragged, and some dying from Covid-19 in the process. The stories were a siren call for me, and I called my old travel recruiter. The last time I’d travelled was 11 years ago, when I went out to San Diego and stayed. I really just wanted to shoot the breeze and get a feel for what was going on, but an hour after talking with her on the phone and sending her an updated resume, I had an offer, and it became real. I went through all of the machinations of getting my ACLS and BLS up to date, applying for a NY license, doing a mountain of paperwork, and the ordeal of making the necessary arrangements through my work. They were reluctant to let me go, and didn’t even have a policy in place for such a leave of absence. I figured out a place to stay, flights, and did some recon work about the neighborhood. From the time I made the first inquiry to my arrival in NYC, it was a week and a half! My husband was worried that I was going to get exposed to Covid and die. He kept it to himself, but I was able to wheedle it out of him. Leaving my 7 and a half year-old son who is very dependent on me was going to be the worst. I felt beyond torn.
I fully expected to get run into the ground here. I was afraid I’d have to fight for PPE, and that once I had it on, that I’d pass out running from room to room with 4 or 5 critically ill patients. I was afraid of exposure. I was afraid I’d be rusty in my ICU skills and wouldn’t be able to handle the load. I figured I’d probably lose a ton of weight due to dashing around and not having any breaks. Boy was I wrong about everything! I was completely unprepared for what I did find.
I arrived to find extremely tired but incredibly welcoming staff and management. Instead of being proprietary about being overrun with a bunch of travelers- strangers in their midst, they were friendly, appreciative and helpful. I was amazed at the purposeful overstaffing. Any other hospital (at least that I’ve ever worked at or heard of) would have cancelled those travel contracts the very second the surge began to let up. I’ve never seen managers and administrators so protective of their staff’s well-being. Lip service, sure, but to literally put their money where their mouth is, is unheard of. I have been at my hospital for 11 years, and I wouldn’t know the CNO if she sat down next to me. I met the CNO at NYP on my second day, and her interest in me and in all the staff seemed genuine. The same for the COO. I was blown away that they converted the entire unit to negative pressure. I was grateful to find easily accessible PPE, and that it was not being micro-managed, but that the staff was trusted to be good stewards of it. And now, I am going home far fatter, thanks to first-rate meals being provided three times a day, not to mention the other goodies.
I would like to thank the following:
- The incredible nursing staff and my fellow travelers. I’ve never worked in a more laterally-supportive environment. Not only have you supported me, but it has been inspiring to see how you support each other. Your sense of teamwork is exemplary. The way you have managed to keep your heads in the game at such a high level after enduring so much trauma, is astounding.
- The EVS staff. You put on PPE countless times and risk exposure as much as anyone else, and make this mission of patient care possible.
- The Physical Therapy staff. I’ve never seen a team roll up their sleeves with such gusto, leaping right in with the best imaginable attitude, providing admirably comprehensive care. You are concerned with the patient as a whole, and your dedication shows. My one recovered patient remembered you all by name.
- Karen, the unit secretary, who made sure I had the right N95, lunch and water and even came in with treats on Mother’s Day- her day off. And Karen, you made me laugh.
- Respiratory, for being dedicated patient advocates.
- The PA’s. I’ve never worked in a PA-driven model before, and I absolutely loved it. I asked, you ordered, it got done. Always knowledgeable, accessible and approachable, you are an impressive bunch.
- Natasha and Jess, for reaching out to me, giving me a thoughtful schedule, and being available.
- Esteen, your professionalism, dedication to both staff and patients comes shining through. You clearly value those whom you manage, and it shows. You lead by example, not hesitating to answer a call bell or go into a patient’s room if you see a need. You support staff recognition and you led them like Joan of Arc through an unimaginable crisis.
- Joan and Juan, the culture of an institution starts at the top, and I’ve never witnessed such supportive and accessible administrators. I’ve never seen an administrator who cared enough about the staff to get to know them as individuals, and to go to such lengths to protect them.
The culture at NYP of Lower Manhattan has made a huge impression on me. This experience is one that I will cherish for a lifetime and I’ll bring back what I’ve learned to San Diego. I’ll always regret that I couldn’t have made it here sooner, when the need was at its most acute, but I feel humbled and honored to have been able to help at all, if only in my own small way. You are immensely special, all of you. You are veterans and survivors, and you managed to come out the other side with your grace, humanity, and dedication still intact.
Thank you so much for welcoming me into your fold if only for a short while. I will never forget you.
Best wishes for your safety and good health,
Rebecca Sauer, RN CPAN
And now, in 36 hours, I’m going home. It’s time. I feel proud of myself for what I’ve done here. I’m glad I got to have an adventure. It’s a good thing.
Tomorrow I’ll do laundry and rest up. I’ll have to leave for the airport at 5am. I started out this journey singing Simon and Garfunkel. And now I’ll finish it with the same. “Homeward Bound.”
Homeward bound
I wish I was
Homeward bound
Home, where my thought’s escapin’
Home, where my music’s playin’
Home, where my love lies waitin’
Silently for me.